February 7, 2019–Shots rang out from a video depicting a chaotic combat scenario, soldiers taking fire while racing through the woods toward a man down, shot in the face and bleeding profusely. Dr. Bob Buckman’s presentation had begun.
February 7, 2019–Shots rang out from a video depicting a chaotic combat scenario, soldiers taking fire while racing through the woods toward a man down, shot in the face and bleeding profusely. Dr. Bob Buckman’s presentation had begun.
A retired trauma surgeon, Dr. Buckman founded Operative Experience Inc. (OEI), a company that has consistently been awarded funding by the U.S. Army and USAID to develop high-fidelity surgical simulators. He believes that combat-relevant training such as that provided by hands-on experience with the true-to-life simulators coupled with rapid trauma skills curricula, provides a complete surgical training system that compares favorably to current programs.
“Simulators provide a means for systematic training that gives medics and surgeons a logical progression for an operation that is much better than the way I was trained,” explained Buckman to a roomful of surgical students, fellows, residents and faculty at the UT Health San Antonio Medical School in late January.
Buckman was a professor of surgery and chief of the trauma service at Temple University Hospital and, subsequently, trauma director at St. Mary Medical Center in Langhorne, PA. He served at the Walter Reed Army Institute of Research during the Vietnam era. Then, as an activated U.S. Army reservist, he cared for hundreds of casualties, mostly Iraqis, at a casualty clearing station and field hospital during Operation Desert Storm. Having unusually extensive experience with penetrating injuries, he had written and lectured widely on their practical management before conceiving of a better way to teach what he knew.
“Medical schools need to do a better job of training residents for combat-relevant wounds,” said Buckman. “I’m very worried about young residents’ ability to perform operations. They are good at taking tests,” he added, “but they are not being asked often enough to prove that they can actually complete the operations they’ll need to do in emergency situations, especially in war-time scenarios.”
His concern is for the entire spectrum of operative experience across the country. Buckman worries that not enough surgeons complete the ATLS program or even the war surgery course, which offers only three days of preparation, before deployment to a war zone. Nor are the other options–ATOM, ASSET or EWSC–sufficient, he believes. Current training methods using animals and cadavers also fall short. “Cutting into a body and into live tissue is different from any other activity—and I believe it needs to be taught.”
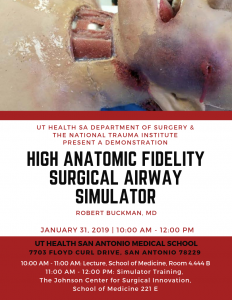
Illustrating his training program in the Johnson Center for Surgical Innovation, Dr. Buckman showed residents and students a brief video pacing through a tracheotomy technique, and then presented them with OEI’s latest simulator: a patient who has sustained a gunshot wound to the face and mouth, drowning in his own blood. The model moved, made noises and spurted blood while, one by one, the UT Health residents practiced the procedure to find the airway, cut through the tissue of the neck, insert a trache tube and balloon below the injury, and pack it to stop the bleeding.
OEI has created simulators and curricula to train surgeons and medics to do craniectomies, laparotomies, amputations, fasciotomies, emergency c-sections and more. “We want the student to be able to DO stuff, not just KNOW stuff,” said Buckman. The goal is to train out mistakes. “This program teaches anatomy, tactics, tools and techniques in a systematic way so that medical personnel who find themselves in tense situations or in austere environments can accomplish the surgery. No one should be out in the field taking care of our soldiers who hasn’t been taught and tested on this stuff.”
With project coordination provided by the National Trauma Institute, OEI’s development of this Airway Simulator was sponsored by the Department of the Army, Prime award W81XWH-15.2.0089. The U.S. Army Medical Research Acquisition Activity, 820 Chandler Street, Fort Detrick MD 21702-5014 is the awarding and administering acquisition office. The opinions, interpretations, conclusions and recommendations are those of the author and are not to be construed as official or as reflecting the view of the Department of the Army or the Department of the Defense.
–Pam Bixby, National Trauma Institute
- Dr. Buckman observes the first resident performing on the airway simulator.
- Attendees discussed follow-on research regarding simulators.
- Dr. Bob Buckman lectures on advances in training simulators.
- A surgical resident at UT Health San Antonio listens intently.
- Dr. Donald Jenkins, Associate Deputy Director of the UT Military Health Institute at UT Health San Antonio, sponsored the simulator demonstration.